
Infective endocarditis presenting as back pain
Introduction
Low back pain is a common and nonspecific complaint including many differential diagnoses at emergency department. Systemic embolization is an unfortunate sequel of infective endocarditis (IE) that can occur despite an appropriate therapy. We present a low back pain patient cause by IE complicated abdominal aortic emboli.
Case presentation
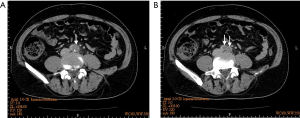
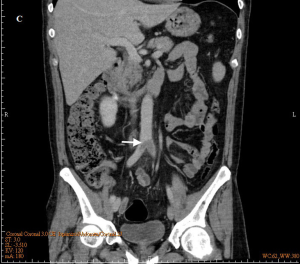
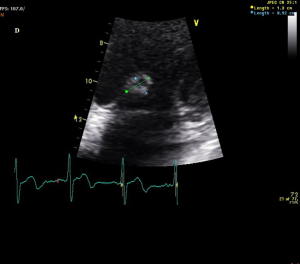
A 51-year-old healthy man presented to emergency department with complaints of severe low back pain for 3 days. He reported a 2-week history of low-grade fever but denied any cough, diarrhea or urinary frequency. His vital signs were normal except body temperature of 37.6 ℃ on arrival. Physical examination revealed only a grade 3/6 systolic murmur, neither peritonitis nor flank knocking pain. Laboratory data showed a white cell count of 14,100/uL, hemoglobin of 11.1 g/dL, microhematuria of RBC 48 cells/HPF and C-reactive protein of 15.6 mg/dL, but others were unremarkable. Abdominal computed tomography (CT) with/without contrast was ordered by an experienced emergency physician because of persistent back pain with fever up to 38 ℃, and it showed a huge aortic thrombus at the level of aortic bifurcation (Figures 1,2, arrows). CT angiogram revealed extensive thrombosis from the left iliac artery to femoral arteries. Transthoracic two-dimensional echocardiography showed a vegetation (1.3 cm × 0.9 cm) at anteromedial leaflet of mitral valve (Figure 3), and severe mitral regurgitation. Blood cultures reported Viridans streptococci. IE was diagnosed. He was treated successfully with broad-spectrum antibiotics and arterial embolectomy with mitral valve replacement.
Discussion
IE is an infection of the heart valves and often causes valvular vegetations. Clinical presentations of IE are often nonspecific and highly variable. A heart murmur is the most commonly physical finding of IE; extra-cardiac manifestations are due to arterial embolization of fragments of the friable vegetation. Large vegetations on the mitral valve, especially on the anterior leaflet, are associated with a higher risk of embolism. Emboli can occlude essentially any vessel in the systemic or pulmonary arterial circulation. Systemic embolization most commonly occurs in left-sided IE; pulmonic embolization most commonly occurs in right-sided IE. Systemic embolization occurs in 22% to 50% of IE patients; emboli may involve major arteries, mostly affecting the central nervous system, but also other organs (1). Embolization to any major arteries contributing to any symptoms may occur; however, persistent low back pain caused by abdominal aortic emboli has never been reported. Current diagnostic criteria of IE include a careful clinical observation, blood culture and echocardiography (2). Contrast-enhanced CT is a useful tool for evaluation of systemic embolization (3). Successful treatments include early and prolonged antimicrobial therapy, and valve-replacement surgery if necessary (1).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ht.2018.07.01). WHC serves as an Editor-in-Chief of Health Technology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mocchegiani R, Nataloni M. Complications of infective endocarditis. Cardiovasc Hematol Disord Drug Targets 2009;9:240-8. [Crossref] [PubMed]
- Li JS, Sexton DJ, Mick N, et al. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000;30:633-8. [Crossref] [PubMed]
- Mylonakis E, Calderwood SB. Infective endocarditis in adults. N Engl J Med 2001;345:1318-30. [Crossref] [PubMed]
Cite this article as: Lin YH, Chang WH, Tsai W, Chien DK. Infective endocarditis presenting as back pain. Health Technol 2018;2:3.


