
Removal of cosmetic oral mucosal tattoos with Nd:YAG laser—histological and clinical observations
Introduction
The cosmetic intraoral tattoos consist of insoluble ink particles injected in subepithelial connective tissue and ingested by phagocytic cells. These phagocytic cells do not remove the tattoo ink away from the mucosa and remain relatively stable. Intraoral tattoos can be divided into amateur and professional. Amateur tattoos usually contain carbonaceous material from Indian ink, charcoal, or magnetite. They are injected into mucosa and usually take the form of relatively simplistic linear lettering or designs. There is usually less particulate matter than in a professional tattoo but the depth of the tattoos may vary more in an amateur tattoo. Professional tattoos can consist of a variety of inks and color using insoluble metal salts and organic complexes. They may be densely colored and occupy small areas of the oral mucosa. The preferable site for oral tattoos is inner labial mucosa.
Despite the paucity of published data, mucosal lip tattooing is not a new phenomenon. The uses of intraoral deposition of exogenous pigmentation are diverse, ranging from gang identification to expressions of love (Figure 1). However, the orolabial mucosal tattoos occur infrequently (1) and because they are hidden, the social stigma that may be associated with traditional tattoos is less of a motivating factor for removal. Unexpected break-ups, changes in lifestyles, and similar reasons are frequently to blame. A number of treatment modalities to remove tattoos could be used by analogy with the dermal tattoos, including surgical excision with grafting, mucobrasion, laser ablation and cryotherapy (2-4). All these treatments result in scarring and tissue deformities to some degree (2-4).

The development of infrared lasers has revolutionized the ability to remove tattoo pigment effectively with minimal scarring and is now widely considered the criterion standard treatment option for skin tattoos. In laser tattoo removal, selective photothermolysis permits the selective destruction of tattoo pigment with very limited damage to surrounding tissue (4). The long-wavelength infrared light of the Nd:YAG laser penetrates deeply (2–6 mm) into skin. Blue or black pigments like melanin enhances Nd:YAG absorption, whereas pale colors enhance its penetration. Although dark pigmented tattoo particles absorption is still poorly studied (different size and color) there is a preferential absorption of the Nd:YAG radiation sufficient to produce changes due to selective photothermolysis (4).
Despite the oral localization of inner lip tattoos, the dentists are not familiar with both the problem and the possibilities to use laser for oral mucosa tattoo treatment. The first and only known report of successful Nd:YAG Q-switched laser removal of professional orolabial mucosal tattoos is published in 2011 by team of dermatologists —Kirby et al. (5). The primary wavelength of this laser is 1,064 nm. The authors reported for three patients with oral tattoos that responded exceptionally well to Nd:YAG Q-switched laser treatment. The suggestion of the authors is that Q-switched laser treatment is a safe and very effective means of removing cosmetic mucosal tattoos on the inner lip and they considered Nd:YAG laser as standard treatment option in this scenario. However the authors generally stated the philosophy of laser treatment in cosmetic dermatology with minor reference to oral mucosa and its specificity. Additional there is no relevant histological data regarding effects of Nd:YAG laser on oral mucosa after tattoo removal procedures. The aim of this publication is to provide histological evidences for possibilities to remove successfully oral mucosa tattoos using 1,064 nm wavelength laser.
Methods
Study design
In 2016 after approval by the Ethics Committee of Medical University of Plovdiv and written consent, a test treatment of five patients with professional black tattoo of inner lip was performed with multi-wavelength laser (Delta Cube laser, Erma Electronique, France) under local anesthesia. The clinical procedure was conducted using 1,064 nm wavelength. Power output of 2 W/20 kHz was applied (4 mm spot size and a fluency of 9.2 J/cm2) for few seconds to discolor the half of tattoo contour. Blanching was achieved by aiming the laser in a moving pattern in a focused mode (Figure 2). Follow-up and photo documentation occurred at intervals from two week till two months. The procedures were repeated twice at interval of two months.

To obtain detailed information about the possible tissue alterations, two equal specimens were taken from the treated and non-treated sites for further histological evaluation (Figure 3). Each biopsy specimen was fixed in 10% buffered formalin, embedded in paraffin and then stained with Hematoxylin and Eosin and Trichrome (for selective demonstration of collagen fibers).

Results
Post-treatment recovery was uneventful, with little pain and swelling. Twelve months after the final procedure almost invisible scarring were observed in all patients but the mucosa color and texture were found normal.
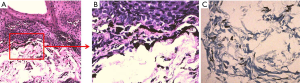
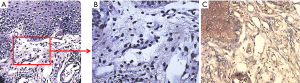
Histologically, the specimens before the treatment showed aggregates of ink particles presented within basal cells and fibroblasts (Figure 4A,B), predominantly in a perivascular location and surrounded by collagen fibers (Figure 4C). Tattoo particles had a mean diameter of 3.52 µm. The specimens after the treatment revealed fragmentation of black ink particles up to 1.5 mm below the surface (Figure 5A,B). Tattoo pigment was progressively altered initially appearing as sharp-bordered grains of pigment in clumps and assuming a progressively amorphous form and lighter color after treatment. Mild fibrosis was seen in the superficial submucosal area where collagen fibers replaced the pigment-containing tissue altered by the laser (Figure 5C).
Clinically, the treatment results showed excellent recovery of the oral mucosa. One year later, the tattoo areas were healthy and without esthetical and functional disturbances (Figure 6).

Discussion
Different wavelengths have been used for selective removal of tattoo in dermatology (6). For example, Q-switched ruby (694 nm wavelength) at 6–8 J/cm2, and Q-switched alexandrite (755 nm wavelength) at 4–8 J/cm2, and Pulsed dye laser (510 nm wavelength) at 3 J/cm2 have been used in removing tattoos. Currently the Nd:YAG laser (1,064 nm wavelength) is considered as golden standard in tattoo removal in dermatology. The primary disadvantage of the 1,064 nm wavelength is the limited color range, which is basically restricted to black and dark blue/black tattoo pigment. However the oral tattoos are predominantly dark colored. The proposed mechanism is that the tattoos pigments absorb the laser energy and this produces very high light intensities up to gigawatts. Inside the pigments, this light is converted into heat within nanoseconds, producing an increase in temperature above 1,000 °C (photothermal effect). This rapid thermal expansion produces shock waves and a potential localized cavitation, so called photoacoustic shock which leads to a particle fragmentation and selective death of pigment containing cells. There is also at the same time a breaking in the chemical bonds inside the pigment (photochemical effect) (4,5,7).
There are no previous reports on histological changes after laser-assisted tattoo removal of oral mucosa. The available analysis of the Nd:YAG laser-induced changed in dermal tattoos has been done by light and/or electron microscopy (8,9). Biopsy of treated tattoos revealed fragmentation of tattoo particles. Little, if any, fibrosis was observed in the superficial dermis. Kilmer et al. (9) noted that despite initial tissue alteration, the lack of both clinical scarring and histologic scarring is most likely attributable to the lack of thermal injury to collagen. The dermis and the epidermis sustain mechanical injury from the photoacoustic wave, but this trauma is apparently highly reparable. Textural changes generally resolve within 4–6 weeks, suggesting an optimal treatment interval of 6 weeks or longer. The majority of patients show no evidence of severe fibrosis or granulomatous change in the late postoperative period. The thinner non-keratinized and well vascularized oral mucosa enable better penetration and suggested more significant thermal effects. Our histological observation are similar to the findings of other authors, however signs of mild fibrosis were evident (6,8). The histologic clearing correlated with clinical clearing of pigmentation where the fibrosis observed histologically does not interfere with the functional and esthetics results.
However laser tattoo removal is uncomfortable. Depending on the patient’s pain threshold, some form of local anesthesia is required. Pre-treatment might include the application of an anesthetic gel under occlusion for 5–10 minutes prior to the laser treatment session. A better method is infiltrative anesthesia which can be administered locally by injections of Ubistesin (articaine hydrochloride 4% with epinephrine 1:200,000). Treatments are repeated at 4- to 8-week intervals, with two to three treatments necessary depending on density of tattoo pigmentation and patients' expectations. Side effects with the Nd:YAG laser are rare and includes transitional swelling, erythema, pinpoint bleeding, pain sensation (10). The incidence of textural change is less than with the other methods. More reaction occurs early in a course of treatment because of the density of pigment and lower fluences for the first one or two treatments can minimize this. The largest spot size available (4 mm) is used with fluence of 9.2 J/cm2. Small spot sizes and higher fluences are more likely to produce pinpoint bleeding. Immediately after treatment there is a greyish discoloration of the area. Healing usually proceeds uneventfully, with discoloration fading after 7–14 days.
Conclusions
As tattooing is becoming more and more popular there is an increasing amount of people requesting tattoo removal. Although inner lip tattoos are still rare, it is conceivable that, as tattoos become more prevalent, the desire to remove them, including those located on mucosal membranes, will increase as well. Within the last decade, Nd:YAG lasers have significantly improved the effectiveness of tattoo removal. The histological studies provided new information and we can better understand the mechanisms of pigment elimination. This publication contributes our knowledge with histological evaluation of Nd:YAG laser removal of professional orolabial mucosal tattoos. It is the contention of the authors that Nd:YAG laser treatment is a safe and very effective means of removing cosmetic mucosal tattoos on the oral mucosa and should be considered the criterion standard treatment option in this scenario.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: GT and JHK serve as an unpaid editorial board members of Health Technology from Sep 2017 to Aug 2019. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study has been reviewed by the Ethics Committee of Medical University of Plovdiv and has been performed in accordance with the ethical standards laid down in the Declaration of Helsinki (as revised in 2013). All persons gave their informed consent prior to their inclusion in this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Laumann AE, Derick AJ. Tattoos and body piercings in the United States: a national data set. J Am Acad Dermatol 2006;55:413-21. [Crossref] [PubMed]
- Clabaugh WA. Tattoo removal by superficial dermabrasion. Five-year experience. Plast Reconstr Surg 1975;55:401-5. [Crossref] [PubMed]
- Wheeler ES, Miller TA. Tattoo removal by split thickness tangential excision. West J Med 1976;124:272-5. [PubMed]
- Goldman L, Blaney DJ, Kindel DJ Jr, et al. Effect of the laser beam on the skin. Preliminary report. J Invest Dermatol 1963;40:121-2. [Crossref] [PubMed]
- Kirby W, Chen C, Desai A, et al. Successful treatment of cosmetic mucosal tattoos via Q-switched laser. Dermatol Surg 2011;37:1767-9. [Crossref] [PubMed]
- Lanigan SW. Lasers in dermatology. London: Springer-Verlag, 2000.
- Choudhary S, Elsaie ML, Leiva A, et al. Lasers for tattoo removal. London: Springer-Verlag, 2010.
- Zelickson BD, Mehregan DA, Zarrin AA, et al. Clinical, histologic, and ultrastructural evaluation of tattoos treated with three laser systems. Lasers Surg Med 1994;15:364-72. [Crossref] [PubMed]
- Kilmer SL, Lee MS, Grevelink JM, et al. The Q-switched Nd:YAG laser effectively treats tattoos. A controlled, dose-response study. Arch Dermatol 1993;129:971-8. [Crossref] [PubMed]
- Adatto MA. Laser Tattoo Removal: Benefits and Caveats. Med Laser Appl 2004;19:175-85. [Crossref]
Cite this article as: Tomov G, Voynov P, Bachurska S, Ke JH, Zagorchev P. Removal of cosmetic oral mucosal tattoos with Nd:YAG laser—histological and clinical observations. Health Technol 2018;2:4.


