
Significance of steerable laparoscopic instrument: usability-based evaluation in a simulation model
Introduction
Laparoscopic instrument was invented to assist surgeons in performing laparoscopic surgery. Therefore, the evolution history of laparoscopic instrument always accompanied surgeon’s demand in certain procedures. Back in the early days of laparoscopic surgery, procedures that could be performed depended much on the available but limited tools (1,2). Because simple procedures in open surgery, such as instrument tie, looping and dissection, might become difficult in the settings of laparoscopic surgery. That is the reasons that more and more instrument designs were invented in recent 2 decades (3-7). One example is the instrument proposed by Murphy et al., which was ultrasonically powered (6).
In the following period, another issue gained speculation. In the past, instruments used in surgery were usually reuseable. Repeated use of such instrument requires disinfection procedures. However, there is risk of incomplete disinfection results. In order to prevent contamination, some forms of disposable laparoscopic instruments were introduced into the market. The overall cost in a procedure using a lot of disposable laparoscopic instrument might be higher than a procedure using a lot of reuseable instrument (8,9). The cost might be as high as two to six folds in the study by the team of Eddie et al. In viewpoint of cost only, reuseable instruments might be more favorable. However, in recent years, the concern of contamination arose again because a newly found disease, prion disease, that can be transmitted through contaminated laparoscopic instruments. The risk of cross contamination is actually underestimated. Although there is always controversy, the final solution is very straightforward, that is using disposable laparoscopic instruments.
The latest trend in laparoscopic surgery is single port laparoscopic surgery (10,11). Because conventional rigid and straight laparoscopic instruments can cause so-called “chopstick effect”, the single port laparoscopic procedure would become extremely difficult and limited. In order to overcome the problem, Yin et al. proposed an instrument with two rotating wrists (11). The design was to assist the operating surgeons to overcome “chopstick effect”. In their initial attempts in 30 patients, the results were favorable and the results demonstrated the safety and efficacy of the design. Wang et al. also developed a design of steerable laparoscopic instruments using four-cable system as transmission to control the end-effectors (12). The team of DragonFlex leaded by Jelinek et al. published a research article about minimizing the rolling joint in their steerable laparoscopic design (13). Their design improved the size and angle of rolling joint in their product, allowing better manipulation during surgery.
In the study, we proposed a novel design of steerable laparoscopic instrument. We test the efficacy of using the instrument and compared the results to that of conventional instrument design. The study is a usability-based evaluation according to MEDDEV revision 4 under directives 93/42/EEC.
Methods
Instrument design
The initial concept is to design an instrument that can exert a full range-of-motion action. During developmental stage of the instrument, there are some limitations in materials and mechanical strength of each structure. The design process was using 3D simulation first and then tested each critical component by making sample components to ensure the strength and function. After repeated tests of the critical components, the required strength and function can be confirmed by the process. The major materials of the hand-held part were made of plastic materials, inclusive of acrylonitrile butadiene styrene and polycarbonate, and the materials providing mechanical strength were made of stainless steel. Both of the materials were safe in terms of biocompatibility and current technology of disinfection by ethylene oxide. The 3D simulation is shown in Figure 1A,B. The product appearance had been optimized for proper handling. The finalized prototype of such instrument is shown in Figure 1C,D.

The basic functions of the steerable laparoscopic instrument included 360-degree rotation of the whole shaft (Figure 2A), articulation of the shaft (Figure 2B) and independent rotation of the end effector (Figure 2C). With all independent functions of the three-axis, the instrument can be used in all directions and can provide more degree-of-freedom during laparoscopic surgery. The mechanical strength of the articulation joint is more than 4 kg during stress test, which is strong enough under most common circumstances. The outer diameter is 4.5 mm, which is compatible with current instrument design and commonly used trocar system. The instrument is insulated in order to connect to an external electrosurgical generator. It can withstand at least 1,200 KV. Before proceeding to the simulation test, the prototype was tested for various scenarios to ensure the strength and safety.

Simulation test
The simulation test is designed based on the requirement of IEC62366 from opening of the package, using the product in common use scenario, worst case scenario, and discarded the product. The scenarios included common use scenario and worse case scenario. The study protocol is shown in Figure 3. The study was performed in the clinical skill center in Tamsheui branch of Mackay Memorial Hospital. The study room is an isolated room with an observable double mirror. The personnel can stand in front of the double mirror to observe, to record and to instruct the tested steps. We used a simulation box to allow surgeons to test for the specific task in each step. The tested procedure included moving a plastic tube in straight line, to throw a knot, to suture in a certain site, to place a string in a certain sequence, to cut a specimen, and to open a candy enclosed in a foil. Performing the procedures was tested by using conventional rigid instrument (Figure 4A), by using steerable laparoscopic instrument (Figure 4B) and by using a predicate device in the test (Figure 4C). The time required for the action and relative difficulty would be recorded and analyzed. The difficulty score of performing a certain procedure ranged from 1 to 5 and the scores were defined in Table 1. The score of difficulty using conventional rigid instrument to accomplish a certain task was defined to be 3 (Table 2). SPSS 13.0 was used to test the difference between each the results of using different instruments by the participated surgeons.
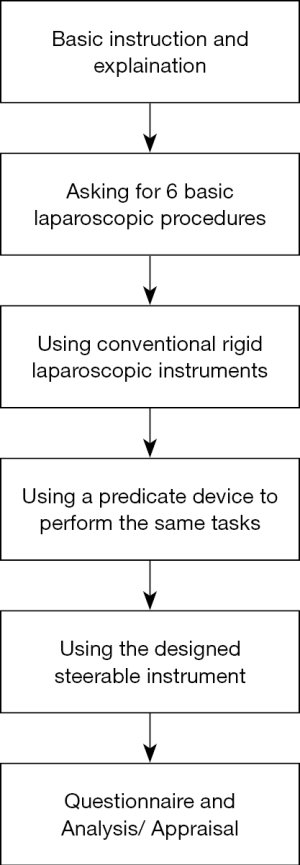

Table 1
| Score | Difficulty |
|---|---|
| 5 | Very easy |
| 4 | Easier |
| 3 | Similar |
| 2 | More difficult |
| 1 | Very difficult |
Table 2
| Surgeon [10] | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Placing plastic tubes | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| Throw a knot | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| Suture | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| Guide a string | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| To cut | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
| Open a candy with foil | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 |
Results
There were ten surgeons involving the usability-based simulation test. The background of the surgeons is showed in Table 3. During the instruction step, the average time required for the surgeons to learn of the operation of steerable laparoscopic instrument and the predicate device, Covidien SILS Clincher, were 3.8 and 4 minutes, respectively. There was no significant difference. All of them can understand the operating principle without reading instruction manual within 5 minutes. All surgeons were quite familiar to conventional rigid instrument and actually there is no time required for them to understand the operating principle. None of the test instruments are broken by wrong manipulation. Therefore, in the worst case scenario, there is no issue of safety concern.
Table 3
| No. | Hospital/specialty | Experience (years) | Handedness |
|---|---|---|---|
| 1 | Medical Center 1/GS | 15 | R |
| 2 | Medical Center 1/GS | 12 | R |
| 3 | Medical Center 1/GS | 10 | R |
| 4 | Medical Center 1/GS | 13 | R |
| 5 | Medical Center 2/GS | 7 | R |
| 6 | Medical Center 2/GS | 2 | R |
| 7 | Medical Center 3/GS | 3 | R |
| 8 | Medical Center 1/GS | 2 | R |
| 9 | Local Hospital 1/GS | 4 | R |
| 10 | Local Hospital 1/GS | 2.5 | R |
GS, general surgery; R, right handedness.
In the simulation test 1, surgeons were asked to use the instrument to move some plastic tubes in a row. In the test, the average score in the steerable laparoscopic instrument is 4.3 and the score in the predicate device is also 4.3. Comparing the two groups, there was no statistical differences. However, the scores of both groups were significantly higher than the score in the rigid instrument group (P value is less than 0.001). The result indicated that using steerable instruments in performing the task is easier than using conventional rigid instrument. In simulation test, surgeons were asked to throw a knot by using different instrument designs. The scores of the steerable instrument were 4.2 and the scores were 4.4 in the predicate device. There was no statistical difference in the two groups. Both scores were significantly better than the scores in conventional rigid instrument group (P value was less than 0.001). In simulation test 3, they were asked to perform an accurate suture in the predetermined site, in the test, the steerable laparoscopic instrument was scored 4.5 in average and the predicate device was scored 4.3, which is quite similar in results. Both of the groups showed better results than the score of conventional rigid instrument. The results demonstrated that using a steerable instrument would be easier for surgeons to perform accurate suturing. In the test 4, surgeons tried to guide a string in certain directions and sequence through metallic hooks. In the test, there were many different directions required to guide the string. Steerable instrument was scored 4.6 and the predicate device was scored 4.5, which were significantly higher than conventional rigid instrument. In simulation test 5, surgeons performed a cutting action in a circular region, the relativity difficulty score in the steerable instrument group was 3.5, significantly higher than the scores in convention rigid instrument group (P value: 0.037), but there was only a borderline trend that the score was better than that of predicate device (P value: 0.598). In the last simulation test 6, surgeons used the instruments to open a candy with foil. The scores were 3.2 in steerable instrument group and 3.3 in the predicate device group. Both scores were not significantly better than the score of conventional rigid instrument group (P value: 0.343). The scores of the proposed instrument and the predicate device are recorded in Tables 4 and 5.
Table 4
| Surgeon | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Placing plastic tubes | 4 | 5 | 3 | 4 | 5 | 4 | 4 | 4 | 5 | 5 |
| Throw a knot | 4 | 4 | 4 | 5 | 4 | 4 | 5 | 5 | 5 | 4 |
| Suture | 4 | 4 | 4 | 4 | 5 | 5 | 4 | 4 | 5 | 4 |
| Guide a string | 4 | 5 | 4 | 4 | 5 | 5 | 5 | 4 | 4 | 5 |
| To cut | 3 | 4 | 3 | 3 | 4 | 3 | 4 | 4 | 3 | 3 |
| Open a candy with foil | 4 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 4 | 3 |
Table 5
| Surgeon | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Placing plastic tubes | 4 | 4 | 5 | 4 | 5 | 4 | 4 | 4 | 4 | 4 |
| Throw a knot | 4 | 4 | 4 | 5 | 4 | 4 | 5 | 5 | 4 | 4 |
| Suture | 4 | 4 | 5 | 4 | 5 | 4 | 5 | 5 | 4 | 5 |
| Guide a string | 4 | 5 | 5 | 4 | 5 | 5 | 4 | 5 | 4 | 5 |
| To cut | 3 | 4 | 3 | 3 | 4 | 4 | 4 | 3 | 4 | 3 |
| Open a candy with foil | 3 | 3 | 3 | 3 | 3 | 3 | 4 | 4 | 4 | 3 |
Discussion
In the history and development of laparoscopic surgery, evolution of surgical instrument plays a great role. In the early days of laparoscopic surgery, surgeons could use some primitive tools or methods to perform laparoscopic surgery. In early days, they were usually simple and uncomplicated procedures (14). Because initial attempts of laparoscopic surgery resulted in promising outcome, more and more demands in instrument emerged (15-17). Delicate and accurate procedure can’t be done without innovative and proper instrument designed for such purpose. The latest trend in laparoscopic surgery can be categorized into two concepts. One concept is to use similar number of port incisions but the incision size is minimized. For example, surgeons can use three 3 mm incisions and one 10 mm camera port instead of four 10mm port incisions to do the same procedures. The main difference is using fine instrument, usually 3 mm in diameter. Instrument of small bore has its own limit in mechanical strength and is usually more suitable in pediatric patients (18). In adult, the application potential of such instrument is quite limited. Another concept is to utilize a single incision, usually umbilical incision, to perform surgical procedures that were previously performed by multiple port incisions. The method is termed as single incision endoscopic surgery (SIES) (19-21). Other terms, such as uni-portal laparoscopy and single port laparoscopy, were indicative of the same concept (22,23). Both concepts have their own advocates.
While performing surgery in either so-called reduced port surgery or SIES, instrument design would influence feasibility and risks of a certain surgical procedure. In the past, some surgeons tried to use conventional rigid laparoscopic instrument to perform SIES. The mode of using instrument in SIES is feasible but usually results in “chop-stick” effect (11,24-26). When the operative space in the abdominal wall created by the incision is small, the middle part of the instrument would be confined in the incision. The hand-held part will interfere with each other and cause difficulty in manipulation of these instruments during a certain procedure. In order to minimize such problem in SIES, there are some potential solutions. The first and simplest solution is to use instruments of different length to minimize interference in the hand-held parts. A demerit of using different length instrument is that there would be some interferences in front effectors (25). A second concept is to use curved instrument to avoid chopstick effects (13). However, curved rigid instrument is not compatible with conventional access device (27-29). Conventional access device is a trocar with long rigid lumen made of plastic materials. When the curve of an instrument is large, it can’t be placed into peritoneal cavity through the access device. A third method is to use instrument that can change direction after entering into peritoneal cavity. Such instrument is termed as articulated instrument or steerable instrument, in a more advanced version. The design of steerable instrument has some advantages. When the instrument is kept in straight line, it could be used as a conventional instrument. When surgeons place the instrument into body cavity, it can be placed through conventional rigid trocar. The shaft can be articulated after the instrument shaft being in the peritoneal cavity. Because selection of certain port incision sites may limit the direction of approach angle of rigid laparoscopic instrument, steerable laparoscopic instrument can provide more degree of freedom during operation.
In our study, we can see that in performing certain tasks by different instrument designs, feasibility of steerable instruments is always better than that of conventional rigid instrument. The only demerit is that users have to learn to use the instrument. Being familiar to certain design may require time and patience for participating surgeons.
The initial simulation study demonstrated that using steerable laparoscopic instrument might be beneficial in performing laparoscopic surgery, especially in SIES. The true benefits and efficacy should be evaluated in an adequate study involving real surgical procedures in the future.
Conclusions
In the usability-based study, we can conclude that using steerable laparoscopic instrument in certain surgical approaches is easier than using conventional rigid laparoscopic instrument. Further study is required to confirm the advantages in clinical setting.
Acknowledgments
Funding: The authors would like to thank the National Taipei University of Technology and Mackay Memorial Hospital, Taiwan for financially supporting this research under Contract No. 108DMH0100070.
Footnote
Conflicts of Interest: CHC serves as an Associate Editor-in-Chief of Health Technology. HCL serves as an unpaid editorial board member of Health Technology from Sep 2017 to Aug 2019. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nordvall S. An instrument to aid laparoscopic diagnosis. Acta Obstet Gynecol Scand 1970;49:111-2. [Crossref] [PubMed]
- Hulka JF. Controlling uterine forceps for laparoscopic sterilization after abortion: a new instrument. Am J Obstet Gynecol 1973;116:884-6. [Crossref] [PubMed]
- Facchin M, Bessell JR, Maddern GJ. A simplified technique for laparoscopic instrument ties. Aust N Z J Surg 1994;64:569-71. [Crossref] [PubMed]
- Dabirashrafi H, Moghadami-Tabrizi N, Zandinejad K. New laparoscopic instrument for removing hair from ovarian dermoid cysts. J Am Assoc Gynecol Laparosc 1994;1:269-70. [Crossref] [PubMed]
- Höferlin A, Höhle KD. Our experience with a new instrument for laparoscopic gallbladder extraction, the "Bergetrokar". Endosc Surg Allied Technol 1993;1:320-1. [PubMed]
- Murphy DL. A new method of laparoscopic instrument knot tying. Surg Technol Int 1995;IV:199-202. [PubMed]
- Miller SS. A new reusable instrument designed for simple and secure knot tying in laparoscopic surgery. Surg Endosc 1996;10:940-1. [Crossref] [PubMed]
- Eddie G, White S. A comparison of reusable versus disposable laparoscopic instrument costs. Aust N Z J Surg 1996;66:671-5. [Crossref] [PubMed]
- Hickey M, Fields M. Laparoscopic cholecystectomy lends itself well to another look at reusable vs. disposable instrument packs. Hosp Mater Manage 1996;21:14-5. [PubMed]
- Msezane LP, Mushtaq I, Gundeti MS. An update on experience with the single-instrument port laparoscopic nephrectomy. BJU Int 2009;103:1406-8; discussion 1408-9. [Crossref] [PubMed]
- Yin H, Wang Z, Xu J, et al. A specific instrument to facilitate single-incision laparoscopic cholecystectomy: an initial experience. Surg Innov 2011;18:289-93. [Crossref] [PubMed]
- Wang X, Wang S, Li J, et al. Conceptual design of a novel multi-DoF manual instrument for laparoscopic surgery. Int J Med Robot 2013;9:75-82. [Crossref] [PubMed]
- Jelínek F, Diepens T, Dobbenga S, et al. Method for minimising rolling joint play in the steerable laparoscopic instrument prototype DragonFlex. Minim Invasive Ther Allied Technol 2015;24:181-8. [Crossref] [PubMed]
- Barnes AB, Welch JP, Malone LJ. Initial experience with laparoscopy for gynecologic patients in a teaching hospital. Report of 100 cases. Arch Surg 1972;105:734-7. [Crossref] [PubMed]
- Lammes FB. The hysterophore: a new instrument for uterine manipulation during laparoscopy. Eur J Obstet Gynecol Reprod Biol 1981;12:243-6. [Crossref] [PubMed]
- Siegler AM. An instrument to aid tubal sterilization by laparoscopy. Fertil Steril 1972;23:367-8. [Crossref] [PubMed]
- Hasson HM. A modified instrument and method for laparoscopy. Am J Obstet Gynecol 1971;110:886-7. [Crossref] [PubMed]
- Loux T, Falk GA, Gaffley M, et al. Single-Incision Single-Instrument Adnexal Surgery in Pediatric Patients. Minim Invasive Surg 2015;2015:246950 [Crossref] [PubMed]
- Raman JD, Cadeddu JA, Rao P, et al. Single-incision laparoscopic surgery: initial urological experience and comparison with natural-orifice transluminal endoscopic surgery. BJU Int 2008;101:1493-6. [Crossref] [PubMed]
- Ohi M, Yasuda H, Ishino Y, et al. Single-incision laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor arising from the duodenum. Asian J Endosc Surg 2013;6:307-10. [Crossref] [PubMed]
- Till H, Metzger R, Woller T, et al. Single incision laparoscopic surgery (SILS) in pediatric urology: decortication of a symptomatic renal cyst in a 14-year-old boy. Eur J Pediatr Surg 2010;20:132-3. [Crossref] [PubMed]
- White WM, Goel RK, Kaouk JH. Single-port laparoscopic retroperitoneal surgery: initial operative experience and comparative outcomes. Urology 2009;73:1279-82. [Crossref] [PubMed]
- Kaouk JH, Haber GP, Goel RK, et al. Single-port laparoscopic surgery in urology: initial experience. Urology 2008;71:3-6. [Crossref] [PubMed]
- Townsend NT, Jones EL, Overbey D, et al. Single-incision laparoscopic surgery increases the risk of unintentional thermal injury from the monopolar "Bovie" instrument in comparison with traditional laparoscopy. Surg Endosc 2017;31:3146-51. [Crossref] [PubMed]
- Balaji S, Singh P, Sodergren MH, et al. A Randomized Controlled Study to Evaluate the Impact of Instrument and Laparoscope Length on Performance and Learning Curve in Single-Incision Laparoscopic Surgery. Surg Innov 2015;22:621-8. [Crossref] [PubMed]
- Sherwinter DA. A novel retraction instrument improves the safety of single-incision laparoscopic cholecystectomy in an animal model. J Laparoendosc Adv Surg Tech A 2012;22:158-61. [Crossref] [PubMed]
- Takayama S, Hara M, Sato M, et al. Initial experience of single-incision laparoscopic right colectomy with minimum umbilical access. Surg Laparosc Endosc Percutan Tech 2011;21:462-3. [Crossref] [PubMed]
- Bracale U, Nastro P, Bramante S, et al. Single incision laparoscopic anterior resection for cancer using a "QuadiPort access system". Acta Chir Iugosl 2010;57:105-9. [Crossref] [PubMed]
- Merchant AM, Cook MW, White BC, et al. Transumbilical Gelport access technique for performing single incision laparoscopic surgery (SILS). J Gastrointest Surg 2009;13:159-62. [Crossref] [PubMed]
Cite this article as: Chen CH, Chang H, Huang TS, Liu TP, Liu HC, Chen CH. Significance of steerable laparoscopic instrument: usability-based evaluation in a simulation model. Health Technol 2019;3:4.


