
Radiographic clue of gas-forming pyogenic liver abscess
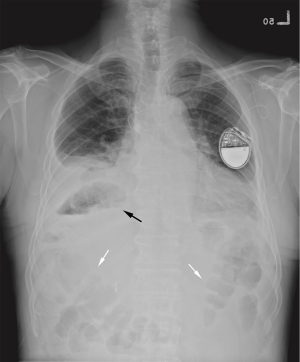
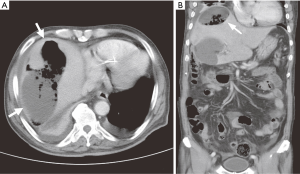
A 79-year-old male patient presented to the emergency room with a history of sick sinus syndrome and pacemaker implantation, single-vessel coronary artery disease, post-percutaneous coronary angioplasty with stent insertion, and diabetes mellitus. He suffered from acute cholecystitis due to gallstones and common bile duct stones. Therefore, he underwent endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy. However, intermittent fever, hyponatremia, and acute renal failure were noted during a 10-day follow-up. His vital signs were as follows: blood pressure of 135/65 mmHg, pulse rate of 65 beats per min, respiratory rate of 20 breaths per min, and core body temperature of 36.4°C. Physical examination of the abdomen revealed normoactive bowel sound and right upper quarter tenderness with rebounding pain. His serum white blood cell count was 20,100 /cumm (reference range, 4,800–10,800/cumm) with left shift, C-reactive protein level was 19.36 mg/dL (reference range, <0.5 mg/dL) and creatinine level was 2.2 mg/dL. (reference range, 0.4–1.2 mg/dL) The chest film (Figure 1) revealed a focal gas collection between the colon gas and right basal lung. Abdominal computed tomography (CT) revealed a gas-forming liver abscess (Figure 2). He received urgent liver abscess drainage, and the pus culture showed the presence of Escherichia coli and Klebsiella oxytoca.
Discussion
Gas-forming pyogenic liver abscess (GFPLA) is uncommon and has an annual incidence rate of 7–24% of all pyogenic liver abscesses. It is associated with a higher mortality rate compared to non-GFPLA. K. pneumoniae is the most commonly associated bacterium with pyogenic liver abscess in Taiwan, especially in patients with GFPLA or diabetic mellitus (1). However, the clinical presentation of GFPLA remains elusive. A combination of fever, right upper quadrant abdominal pain, and hepatomegaly is common but nonspecific. Based upon the lack of specificity of clinical symptoms and laboratory findings, imaging examinations are usually required for accurate diagnosis. The diagnosis of GFPLA depends mainly on ultrasonography and/or CT scan, with confirmation by needle aspiration for bacteriology studies. The therapeutic strategy consists of administration of bactericidal antibiotics, adequate drainage of abscess, and control of the primary source of infection (2).
In our patient, the abnormal air in the liver abscess near the hepatic flexural colon was a clear indication and easily identifiable. The differential diagnosis for gas in the right upper abdomen is broad, and includes intra-abdominal free air, bowel gas displacement, emphysematous changes in the liver and gallbladder, and following invasive procedures (3-5); therefore, physicians should pay attention to this area when reading the radiographic images.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ht.2020.01.01). WHC serves as an Editor-in-Chief of Health Technology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lee HL, Lee HC, Guo HR, et al. Clinical significance and mechanism of gas formation of pyogenic liver abscess due to Klebsiella pneumoniae. J Clin Microbiol 2004;42:2783-5. [Crossref] [PubMed]
- Jun JB. Klebsiella pneumoniae Liver Abscess. Infect Chemother 2018;50:210-8. [Crossref] [PubMed]
- Musson RE, Bickle I, Vijay RK. Gas patterns on plain abdominal radiographs: a pictorial review. Postgrad Med J 2011;87:274-87. [Crossref] [PubMed]
- Grayson DE, Abbott RM, Levy AD, et al. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics 2002;22:543-61. [Crossref] [PubMed]
- Doblecki-Lewis S, Palaios E, Bejarano PA, et al. Hepatic gas gangrene following orthotopic liver transplantation: three cases treated with re-transplantation and a review of the literature. Transpl Infect Dis 2008;10:280-5. [Crossref] [PubMed]
Cite this article as: Liu HT, Chiu YH, Chang WH. Radiographic clue of gas-forming pyogenic liver abscess. Health Technol 2020;4:1.


