Clinical practice review on telehealth for managing a population with chronic urinary tract infections during the COVID-19 pandemic
Introduction
In December 2019, the COVID-19 pandemic caused severe illness and mortalities around the world (1). The shift from conventional clinical practice to socially distanced digital health changed the dynamic of chronic healthcare management to protect the public and minimize the risk of COVID-19 viral transmissions (2). Population health management (PHM) continued to be an essential health infrastructure that relied on collaborative data and interprofessional co-production to manage patients with long term chronic illnesses (3). A chronic urinary tract infection (UTI) is common bacterial invasion of the lower urinary tract, evident among older adults in primary and secondary care (4), and a chronic illness that blighted the lives of many during the COVID-19 pandemic (5). The advances in digital health such as telemedicine, real-time videoconferencing and telephone consultations have supported the continuation of collaborative care management (6), and patients with chronic UTI accompanied with lower urinary tract symptoms have relied upon expert knowledge from an interprofessional approach to manage their bladder condition (7). Calton et al. (8) have highlighted the importance of telehealth during the pandemic, as it helped to reduce the spread of COVID-19 in clinical settings and within local communities. The aim of this clinical practice review was to identify the key successes of telehealth when caring for population diagnosed with a chronic UTI during the COVID-19 pandemic. The RIGHT checklist was used to guide the reporting process of this clinical practice review (9), and provided a systematic structure to ensure keys components of the checklist were incorporated as part of the reporting process.
Methodology
We gathered evidence-based opinions of clinicians and researchers who specialized in the field of chronic UTI. And also included evidence-based perspectives from countries that utilized a PHM approach to manage chronic UTI during the COVID-19 pandemic. This clinical practice review was guided by the following questions, how effective was telehealth during the COVID-19 pandemic for patients with chronic UTI? What are the recommendations for population health management and chronic UTI in the future?
Search strategy
This clinical practice review was constructed using PubMed and CINHAL Plus databases. The search was targeted at the nursing and medical discipline, and the following search terms Population health, Urinary Tract Infection, Urogynecology, LUTS, Telehealth, COVID-19 were inserted into both databases combined with Boolean search operators AND and OR. We searched for publications dated between December 2019 and April 2022 and decided to select all publications that evaluated the use of digital health technologies for managing a population diagnosed with chronic UTI. Table 1 was developed to extract data from the reviewed publications and evaluate the papers for their outcome data, strengths, limitations and the application of PHM for chronic UTI. All of the authors revisited the titles and abstracts of the selected publications to ensure that the papers were selected according to the objectives of the clinical practice review, and to ensure the publications were available in full text to review the findings.
Table 1
| Author/year study published/reference | Country | Study design | Outcome | Strengths and limitations of technology-based care |
|---|---|---|---|---|
| Grimes et al. 2020, (10) | USA | Systematic review and Census study | A critical element of transitioning to telemedicine is maintaining the unique elements of trust, privacy and information-sharing that occur between provider and patient | Strength: telemedicine is effective for uncomplicated follow up appointments. Limitations: limited or no internet access can affect telemedicine follow-up appointments |
| Medina-Polo et al. 2020, (11) | Spain | Comprehensive review of the literature | The diagnosis and prescription of treatment for LUTS and BPH during the COVID-19 pandemic should be based on telemedicine and joint protocols for primary care attention and urology | Strength: promotion of telemedicine and joint protocols for Primary Care. Limitations: clear diagnostics, treatment criteria and referral could be limited |
| López-Fando et al. 2020, (12) | Belgium; Brazil; France; Italy; Portugal; Spain; Turkey; United Kingdom; USA | International narrative review | Efforts should be made to minimize the burden for this patient group, without endangering patients and health care workers during the COVID-19 pandemic | Strength: telemedicine is a method for follow-up cases not requiring a physical examination or other testing methodologies. Limitations: the older population and people who are economically disadvantaged may not have access to health technologies |
| Novara et al. 2020, (13) | Italy | Systematic review on Telehealth and Urological applications | Telemedicine has been implemented successfully in several common clinical scenarios, such as follow-up care, of uncomplicated urinary stones and uncomplicated UTIs | Strength: telehealth is successful for patients diagnosed with uncomplicated LUTS. Limitation: safety concerns for patients with malignant or complex diagnoses |
| Bakhit et al. 2021, (14) | Australia | Systematic review and meta-analysis | Antibiotic prescribing through telehealth for patients with UTI showed no difference in comparison to face to face consultations | Strengths: telehealth consultations during COVID-19 ensured patients had access to primary care services and treatment for diagnosed UTIs. Limitations: telehealth may change the diagnostic process because of the limitations on physical examination |
| Somani et al. 2020, (15) | United Kingdom | 7-week observation of patients attending an outpatient department for LUTS during a national lockdown | COVID-19 virtual outpatient clinics with telemedicine for patients with LUTS and urgent urological surgery can continue to be carried out to minimize disruption to services | Strength: potentially mitigate the impact of delaying patients most in need. Limitation: risk of losing of vital clinical information |
LUTS, lower urinary tract symptoms; BPH, benign prostatic hyperplasia; UTIs, urinary tract infections.
Eligibility criteria
Inclusion criteria
Articles were included if they were peer reviewed papers, with full text access and related to population health, urinary tract infection, urogynecology, LUTS, telehealth, COVID-19.
Exclusion criteria
The publications that did not have direct relevance to the clinical practice review or focused on the related questions were excluded.
Results
Characteristics of included studies
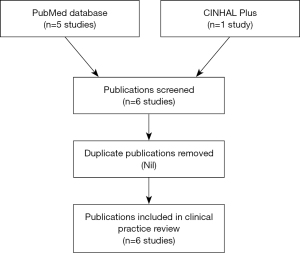
The number of publications retrieved were limited due to the publication dates and the topic being reviewed. A total of five publications were accessed from PubMed and the other publication was obtained from CINHAL Plus. Six papers were selected as they were relevant to the key search criteria and provided data for this clinical practice review. The process of retrieving the literature and selecting the articles included in this review has been illustrated in a flow diagram (Figure 1) which complied with the RIGHT checklist for reporting a clinical practice review. Of the six publications included within this review, five were review papers (10-14) and one was an observational study (15). The authors of the five review papers had evaluated current literature on the effectiveness of telehealth for a patient population group with lower urinary tract symptoms and UTI and expressed the significance of implementing telehealth during the COVID-19 pandemic. The authors from the observational study examined clinical practice during the COVID-19 lockdown period and their implementation of telehealth as part of continued urological services during the pandemic. The findings from their study demonstrated the importance of adapting healthcare delivery and implementing telemedicine during the pandemic for continued patient care.
Discussion
The effectiveness of telehealth
There is evidence that telehealth and digital technology is an accessible method for delivering continued care to patients (16). A recent study has highlighted that a large patient population group are prepared to keep follow up appointments scheduled during the COVID-19 pandemic with the use telehealth (17). The ability to assess, review and design a treatment plan remotely for a population group with a UTI is an advancement in digital health care management. Health technologies are spreading, enabling follow-up consultations and health care management without the need for physical attendance and alleviates the impact of accommodating patients within a health care setting (15). Telemedicine has been regarded as an essential method for patient review and follow-up during the COVID-19 pandemic particularly for LUTS cases secondary to UTI (12). Somani et al. (15) lay emphasis the impact of virtual urological services being the optimal method of minimizing service disruption and Bakhit et al. has shown that telehealth treatment prescribing for UTI does not differ from face to face, and is an effective method of distanced management of the disease (14). Although telehealth has evolved and is a convenient method of managing a population with chronic UTI, challenges may be present in a population who are not digitally competent which is evident through the lack of digital skills, comprehension of how to use health technologies and technophobia (10,12). This poses the risk of inadequate follow-up consultations and a disparity in shared health information (15). A situation which is more apparent in population groups with complex diagnoses (13).
Population health management and chronic UTI in the future
The COVID-19 pandemic highlighted the significance of PHM through collaborative, integrative health care and the use of telehealth for disease diagnosis and continuation of care management (11). Collaborative care with the use of digital health technologies and telehealth was a sustainable method for patient decision-making, diagnosis of chronic UTI symptoms and treatment processes (13). With the steep rise in telehealth during the COVID-19 pandemic (15), the acceptance and integration of telehealth from a PHM perspective advances chronic health care management, health telecommunications and digital technology (10). Patients with chronic UTI have relied on telehealth as an effective method for obtaining treatment and follow-up as well as lowering the clinical demands on health services (18).
Telemedicine has been recognized for minimal disruption to health services and patient care (15), and incorporating it as a health management strategy for managing chronic UTI is essential to continue care for a population group with a debilitating condition (10). There are evidence-based recommendations that highlight the importance of patient assessment, level of engagement and evaluation of telehealth efficacy in long-term telehealth use (19). The reliance on individualized specialist care management for chronic long term illnesses without a collaborative approach and digital health has become past practice, and contemporary PHM for patients with chronic UTI through digital technology has become widely used. Whilst telehealth is a sustainable method for managing populations with chronic illnesses, it is essential that healthcare professionals are adequately trained and competent when using digital health technologies for managing patients with chronic illness. This will help maximize collaborative healthcare delivery without compromising quality health care and safety (15). The COVID-19 pandemic has changed the way healthcare is delivered, and PHM for chronic UTI has seen an advanced uptake of digital health technologies. The available data on telehealth during the COVID-19 pandemic has promoted the use of digital health technology for managing populations chronic illnesses and more so for patients diagnosed with a chronic UTI. The future of telehealth and PHM for chronic UTI is optimistic, as integrative and collaborative healthcare management has advanced as a result of the pandemic and beyond.
Implications for practice
Health care professionals should be prepared to provide integrative and collaborative healthcare with the use of telehealth. Patient engagement with treatment and follow-up using telehealth has been welcomed by various populations diagnosed with chronic illnesses (13). There is evidence that digital health management has been successful and telehealth usage has increased over the past two years (15). Health care professionals could promote awareness of telehealth for patients who are not technologically competent, by delivering educational workshops on the benefits managing their chronic illness through the use of telemedicine.
Limitations
There were limited number of publications retrieved for this clinical practice review, thus may not have given comprehensive insight on the key successes of telehealth when caring for a population diagnosed with a chronic UTI during the COVID-19 pandemic. However, the reviewed papers have highlighted the significance of telehealth when managing a population group remotely who have been diagnosed with a chronic illness.
Conclusions
The available literature on telehealth, population health management and chronic UTI during the COVID-19 pandemic has demonstrated a sustainable and cost-efficient method for managing a population group with a chronic illness. Undoubtedly, there is a need to monitor and evaluate the effectiveness of telehealth within this population group to eliminate information disparities and failed follow-up consultations. It is essential that healthcare professionals are adequately trained on how to effectively use telehealth when conducting consultations and follow-up appointments and evaluate the risks of bypassing patient groups who are not digitally competent to actively participate in telehealth for managing their chronic UTI.
Acknowledgments
The authors would like to thank Dr. Jacqueline Guendouzi, Professor, Department of Health and Human Sciences, Southeastern Louisiana University, for granting assigned time to conduct this clinical practice review.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ht.amegroups.com/article/view/10.21037/ht-22-9/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507-13. [Crossref] [PubMed]
- Figueiredo AA, Fernandes A, Fornari A, et al. Interim Guidance for Urodynamic Practice during COVID-19 Pandemic. Int Braz J Urol 2021;47:178-84. [Crossref] [PubMed]
- Cronin CE, Franz B, Schuller KA. Expanding the Population Health Workforce: Strategic Priorities of Hospital Organizations in the United States. Popul Health Manag 2021;24:59-68. [Crossref] [PubMed]
- Rosello A, Pouwels KB, Domenech DE, Cellès M, et al. Seasonality of urinary tract infections in the United Kingdom in different age groups: longitudinal analysis of The Health Improvement Network (THIN). Epidemiol Infect 2018;146:37-45. [Crossref] [PubMed]
- Reyes R, Bono G, Finucane TE. So-called Urinary Tract Infection in the Era of COVID-19. J Am Geriatr Soc 2020;68:1927-8. [Crossref] [PubMed]
- Buvik A, Bergmo TS, Bugge E, et al. Cost-Effectiveness of Telemedicine in Remote Orthopedic Consultations: Randomized Controlled Trial. J Med Internet Res 2019;21:e11330. [Crossref] [PubMed]
- Medina-Polo J, Adot JM, Allué M, et al. Consensus document on the multidisciplinary management of neurogenic lower urinary tract dysfunction in patients with multiple sclerosis. Neurourol Urodyn 2020;39:762-70. [Crossref] [PubMed]
- Calton B, Abedini N, Fratkin M. Telemedicine in the Time of Coronavirus. J Pain Symptom Manage 2020;60:e12-4. [Crossref] [PubMed]
- Chen Y, Yang K, Marušic A, et al. A Reporting Tool for Practice Guidelines in Health Care: The RIGHT Statement. Ann Intern Med 2017;166:128-32. [Crossref] [PubMed]
- Grimes CL, Balk EM, Crisp CC, et al. A guide for urogynecologic patient care utilizing telemedicine during the COVID-19 pandemic: review of existing evidence. Int Urogynecol J 2020;31:1063-89. [Crossref] [PubMed]
- Medina-Polo J, Téigell Tobar J, Romero-Otero J, et al. Benign prostatic hyperplasia management during COVID-19 pandemia. Arch Esp Urol 2020;73:405-12. [PubMed]
- López-Fando L, Bueno P, Carracedo D, et al. Management of Female and Functional Urology Patients During the COVID Pandemic. Eur Urol Focus 2020;6:1049-57. [Crossref] [PubMed]
- Novara G, Checcucci E, Crestani A, et al. Telehealth in Urology: A Systematic Review of the Literature. How Much Can Telemedicine Be Useful During and After the COVID-19 Pandemic? Eur Urol 2020;78:786-811. [Crossref] [PubMed]
- Bakhit M, Baillie E, Krzyzaniak N, et al. Antibiotic prescribing for acute infections in synchronous telehealth consultations: a systematic review and meta-analysis. BJGP Open 2021;5. BJGPO. [Crossref] [PubMed]
- Somani BK, Pietropaolo A, Coulter P, et al. Delivery of urological services (telemedicine and urgent surgery) during COVID-19 lockdown: experience and lessons learnt from a university hospital in United Kingdom. Scott Med J 2020;65:109-11. [Crossref] [PubMed]
- Gadzinski AJ, Gore JL, Ellimoottil C, et al. Implementing Telemedicine in Response to the COVID-19 Pandemic. J Urol 2020;204:14-6. [Crossref] [PubMed]
- Boehm K, Ziewers S, Brandt MP, et al. Telemedicine Online Visits in Urology During the COVID-19 Pandemic-Potential, Risk Factors, and Patients' Perspective. Eur Urol 2020;78:16-20. [Crossref] [PubMed]
- Mehrotra A, Paone S, Martich GD, et al. A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med 2013;173:72-4. [Crossref] [PubMed]
- Sacco E, Gandi C, Li Marzi V, et al. Extensive impact of COVID-19 pandemic on pelvic floor dysfunctions care: A nationwide interdisciplinary survey. Neurourol Urodyn 2021;40:695-704. [Crossref] [PubMed]
Cite this article as: Collins L, Uzoaru F, Khasriya R. Clinical practice review on telehealth for managing a population with chronic urinary tract infections during the COVID-19 pandemic. Health Technol 2022;6:2.